Researchers in a study recently published in the journal Gut investigated the involvement of gut bacteria in food addiction-related processes.

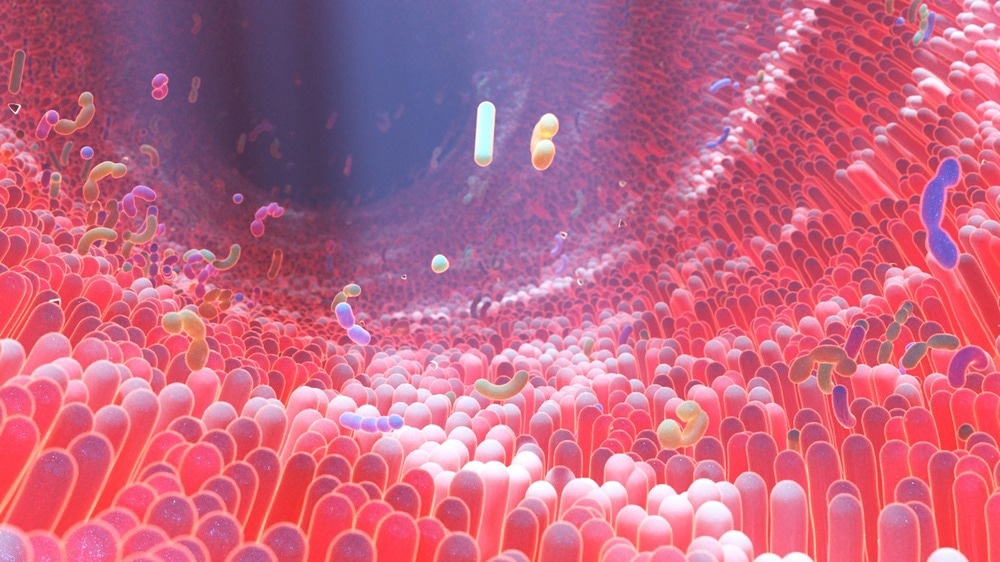
Study: Gut microbiota signatures indicative of vulnerability to food addiction in mice and humans. Image credit: Alpha Tauri 3D Graphics/Shutterstock.com
background
Uncontrolled food intake can lead to obesity and altered gut bacteria. Brain changes associated with behavioral disorders affect the gut microbiome, and gut bacteria affect brain regions involved in behavioral control.
Recent research into gut microbiota profiles associated with addictive diets has generated interest, but studies have been primarily focused on rodents, highlighting the paucity of translational research using animal models to confirm human findings.
About the Research
In this study, the researchers investigated the functional role of gut bacteria in food addiction and uncontrolled eating.
C57Bl/6J mice underwent an operant food addiction procedure with six reinforcement sessions using a fixed ratio (FR) of 1 and 92 regular sessions of FR5. Researchers used the Yale Food Addiction Scale (YFAS) to assess food addiction in mice and humans.
By feeding them non-digestible carbohydrate types such as rhamnose and lactulose and examining the fecal microbiota, the researchers functionally confirmed the importance of Blautia microbes, which were most differentially expressed between the intoxicated mouse and human populations.
The researchers also used quantitative polymerase chain reaction (qPCR) gene expression in mouse food addiction technique to validate its functionality in Blautia therapy.The genes evaluated included dopamine receptor type 1 (DRD-1), DRD-2, tyrosine hydroxylase, and dopamine and cyclic adenosine monophosphate-regulated neuronal phosphorylation protein (DARPP-32).
The researchers orally administered Blautia wexlerae at a dose of 1.0 × 109 colony-forming units to mice enduring a long-term food addiction protocol for 3 days per week. They used 16S ribosomal ribonucleic acid (rRNA) sequencing of cecal contents to detect gut microbial profiles associated with uncontrolled feeding behavior.
The researchers used principal component analysis (PCA) on key variables such as persistence of response, compulsion, motivation, withdrawal, tolerance, distress, and appetite. Correlation assessments allowed for a simultaneous display of mouse and human addiction criteria.
Additionally, the researchers used correlation matrices to explore the relationship between each addiction criterion and each phenotypic trait in the mouse and human populations. Covariates in the study included age, body mass index (BMI), and biological sex.
result
The study identified gut microbiome patterns as prospective biomarkers for food addiction. The gut microbiome profiles associated with food addiction were remarkably similar between the mouse and human groups.
The findings suggested that Proteobacteria may have a negative effect on the development of food addiction in mice and humans, while Actinomycetes may have a protective effect.
The researchers found that the relative abundance of Blautia wexlerae was low among poisoned humans and the abundance of the genus Blautia was low among poisoned mice. Rhamnose and lactulose, which promote the growth of Blautia, increased the abundance of Blautia in the feces of mice and significantly improved food poisoning. The team found that a similar improvement was observed after administration of the beneficial microbe Blautia wexlerae.
The mouse cecal microbiota was dominated by the phyla Firmicutes and Bacteroidetes, accounting for approximately 90% of the relative abundance in toxigenic and non-toxigenic animals. Certain bacteria, such as Actinobacteria, Erysipelotrichaceae, Coriobacteriaceae, Enterohabdus, and Lachnospiraceae, were shown to be less abundant in toxigenic mice than in non-toxigenic mice.
Genus-level analysis showed that the genera Ruminococcaceae and Gastranaerophilales were positively correlated with motivation in intoxicated mice, whereas Lachnospiraceae, Ruminococcaceae, Candidatus arthromitus, Peptococcus, Ruminiclostridium_6, Acetatifactor, Coprococcus_1, and Roseburia were positively correlated with response persistence in intoxicated mice.
Diet composition had little effect on gut microbiome data. In mice, rhamnose-fed mice showed much lower desire for chocolate-flavored pellets than lactulose-fed mice, demonstrating that non-digestible carbohydrates help avoid food addiction. Animals receiving Blautia showed the same persistence of response, but showed much lower desire and compulsion for the attractive food than control mice.
In food-intoxicated conditioned animals, the abundance of many essential bacterial groups was decreased, suggesting a possible protective effect. In contrast, the relative abundance of the Anaeroplasmagenus and Gastranaerophilales families was increased in intoxicated mice, suggesting an unfavourable effect.
Findings indicate that an increased relative abundance of the genus Enterorhabdus (Actinobacteria) in the gut of non-addicted mice may be advantageous, and that the genus Lachnospiraceae in the phylum Bacillota or Firmicutes may have a favorable effect on food addiction, consistent with previous studies. qPCR analysis showed non-significant differences in gene expression in key regions of the reward system, such as the nucleus accumbens (NAc) and medial prefrontal cortex (mPFC), between mice treated with Blautia.
Conclusion
Findings suggest a link between gut microbiota and risk of food addiction. Gut microbiota composition was associated with key addiction traits, including motivation and persistence of response. Blautia, a non-digestible carbohydrate, was functionally relevant and effective in preventing the development of food addiction in rats.
The findings suggest that the gut microbiota may predispose people to food addiction and could lead to new technologies for creating biomarkers and new treatments for uncontrolled eating and related disorders.