Although hair loss can be painful and devastating, it isn’t considered a serious health issue. As a result, there are relatively few biotech companies tackling it. One of them is Stemson Therapeutics, which is pioneering hair regeneration using induced pluripotent stem cells (iPSCs). The company says its iPSC-based approach is good enough to meet the huge market demand for solutions to cicatricial alopecia, male pattern baldness, and chemotherapy-induced alopecia.

“Tissue degeneration, which manifests as hair loss, means that the cells responsible for hair production die,” says Stemson CEO Jeff Hamilton. “The logical approach is to replace or regenerate those lost cells, and that’s where stem cells come in.”
Some scientists have tried culturing cell populations derived from adult hair follicles to generate transplant material, but that approach has not been particularly effective. Stemson is taking a different approach, relying on iPSCs. “iPSCs offer us a better, more reliable, robust, and scalable way to generate a source population of highly specialized cells needed for hair follicle growth,” Hamilton argues.
Hamilton cautions that Stemson’s approach is currently in preclinical development and still needs to be tested in humans. That means there will be years of development before the treatment can enter human trials, and years before it’s available, even if it’s successful. “The science we’re doing is so novel that no one can predict exactly when it will be ready for clinical trials,” he adds.
When clinical trials eventually begin, they will evaluate first-generation autologous transplant treatments, “which are simpler and have fewer clinical risks,” Hamilton said. “In the longer term, we also plan to develop a more cost-effective allogeneic transplant approach.”
Procedural details
“Today’s hair transplant surgery is a two-step procedure that begins with the excision of the hair-containing donor tissue (usually 1mm-sized punches),” Hamilton points out, “These punches are then inserted into the same-sized punch areas of the recipient.”
Stemson’s procedure skips the excision step and starts by extracting somatic cells from the patient (such as blood or skin cells) and reprogramming them into iPSCs, which are then amplified and differentiated into hair follicle germ layer and then prepared for transplant into the patient.
“As the insertion site heals, the tissue becomes vascularized, which is essential for nourishing the hair matrix cells,” Hamilton explains. “The hair matrix cells form hair follicles, whose cells begin to multiply and grow from deep within the implantation site into the surface skin tissue.”
The process is similar to planting a seed in a garden, with one big difference: Stemson’s method requires that the pores remain open during the healing process to allow the hair shaft to emerge from the skin. This is achieved using tiny biodegradable scaffolds, or placeholders, similar to the material used in surgical sutures. “It takes two months for the hair to emerge,” says Hamilton.
Male pattern baldness occurs because the biochemical environment destroys and damages hair follicle tissue, especially the dermal papilla components. But that environment may not be as damaging to newly transplanted hair matrix cells. “Because hair matrix cells are like newborns, they’re less susceptible to biochemicals that damage the dermal papilla of the hair follicle, such as dihydrotestosterone (DHT),” Hamilton explains. When new hair follicles form, their clean, natural environment should offer some protection from those biochemicals.
Clinical trials will need to determine whether and for how long that protection lasts in humans. To further improve the chances that hair will grow and follicles will remain healthy, Stemson plans to evaluate naturally resistant follicles to identify their key protective properties. The company may use these findings to guide hair germ selection.
Family Support
Stemson was founded when a father and son wanted to work together on a project that combined their talents. Co-founder and CSO Dr. Alexey Terskikh is a scientist at the Sanford Burnham Prebys Medical Discovery Institute who has spent most of his career researching stem cells and regenerative medicine. His father is a biologist who studies skin. They decided to seize the opportunity to work together on generating new dermal papilla cells.
“They were the first to differentiate iPSCs into dermal papilla cells,” Hamilton notes. “Once the human dermal papilla cells differentiated into mouse hair follicles, father and son realized that this could create an attractive commercial opportunity.” Hamilton joined Alexei Terskikh to found Stemson in 2017.
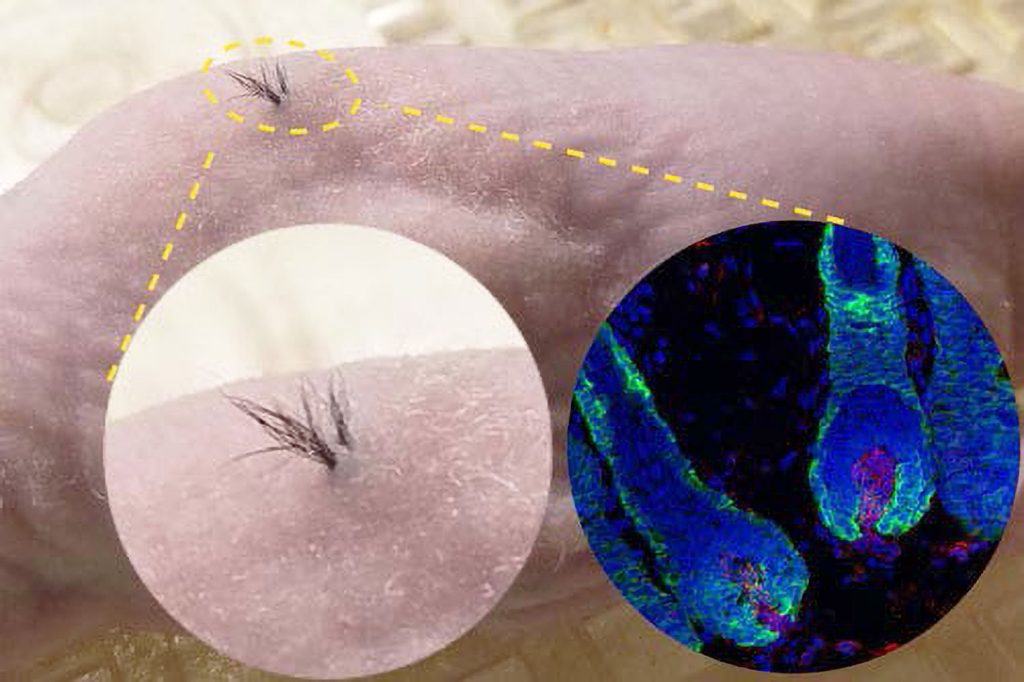 Stemson Therapeutics is using mouse models for preclinical development and has begun employing a pig model. In this image, nude mice are implanted with human iPSC-derived dermal papilla cells and mouse epithelial cells within a biodegradable scaffold. Left inset: Magnified view. Right inset: Fluorescence microscopy image of a hair follicle beneath the skin (blue: cell nuclei, green: epithelial cells, red: human dermal papilla cells).
Stemson Therapeutics is using mouse models for preclinical development and has begun employing a pig model. In this image, nude mice are implanted with human iPSC-derived dermal papilla cells and mouse epithelial cells within a biodegradable scaffold. Left inset: Magnified view. Right inset: Fluorescence microscopy image of a hair follicle beneath the skin (blue: cell nuclei, green: epithelial cells, red: human dermal papilla cells).
The company faced two big challenges early on. “The first was investment,” Hamilton recalls. “There’s an embarrassingly small amount of industry money invested in hair loss treatment. Companies rarely make it part of their strategy.” With the exception of Allergan, one of Stemson’s early investors.
“The second challenge was building a strong scientific team,” Hamilton continues. “Very few people focus their biological research and careers on treating hair loss.”
Scientific Challenges
Hamilton says the company has now overcome those hurdles. Now, the challenge is scientific. “Hair follicles are very complex little organs that contain many cell types working together,” he explains. “How to combine these cell types to drive hair follicle development and to make the follicle survive transplantation into a complex organism is a challenge.” Stemson’s team is looking at variables, control, timing issues, and strategies to manufacture different hair follicle components.
Another challenge, he says, is finding a suitable experimental model: “Most treatment development is done in mice, but what you see in mice doesn’t necessarily translate to humans.” The team expects that pigs will be able to more accurately mimic the human skin environment.
If this method works in humans, it would be an absolute breakthrough, allowing new hair to grow permanently rather than temporarily. “This is the first ever delivery of new hair follicles,” Hamilton declares. He suggests that even bald people could potentially regrow their hair using the treatment.
According to Hamilton, minoxidil is a band-aid approach: “It temporarily stimulates the hair to grow some of the remaining stem cells into hair follicles, but it doesn’t prevent the long-term degeneration of the hair follicles,” he claims. “Eventually, it stops working because there aren’t enough hair follicle cells left.” Propecia (finasteride), which is often used in conjunction with minoxidil, attempts to halt further hair loss, but doesn’t prevent degeneration.
Stemson’s iPSC technology appears to be scalable, meaning it could potentially generate as many hair follicles as needed for each patient.
The company is now focused on completing research and development work — “we need to demonstrate that our solution works consistently in pigs,” Hamilton says — after which Stemson will need to raise additional funding to move forward with clinical trials.